Diferencia entre revisiones de «Intestino Delgado - Resumen - Anatomía & Fisiología»
| (No se muestran 8 ediciones intermedias del mismo usuario) | |||
| Línea 1: | Línea 1: | ||
| − | == | + | ==Introduction== |
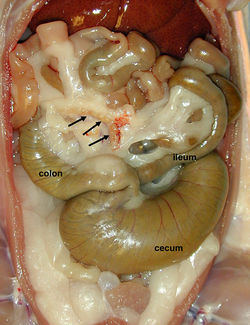
| − | + | The small intestine extends from the pylorus of the [[Estómago Monogástrico - Anatomía & Fisiología|stomach]] to the [[Ciego - Anatomía & Fisiología|ciego]]. The small intestine recieves chyme from the [[Monogastric Stomach - Anatomía & Fisiología|stomach]]. It is the main site of chemical degradation and absorption of chyme. Fats are exclusively broken down in this part of the alimentary tract. Carbohydrates and proteins that are not degraded in the small intestine are available for microbial fermentation in the [[Intestino Grueso - Anatomía & Fisiología|intestino grueso]]. The small intestine produces enzymes for digestion of protein, carbohydrate and fat and absorbs the products of their digestion. Enzymes are produced by glands in the intestinal wall and the [[Páncreas - Anatomía & Fisiología|páncreas]]. The [[Vesícula Biliar - Anatomía & Fisiología|vesícula biliar]] produces bile which emulsifies fats for digestion. Absorption is facilitated by ridges in the small intestine and by the presence of villi and microvilli. | |
| − | + | The small intestine consists of three parts. Each part differs in anatomy, but all have the same basic structure and function: | |
*[[Duodeno - Anatomía & Fisiología|Duodeno]] | *[[Duodeno - Anatomía & Fisiología|Duodeno]] | ||
*[[Yeyuno - Anatomía & Fisiología|Yeyuno]] | *[[Yeyuno - Anatomía & Fisiología|Yeyuno]] | ||
| − | *[[ | + | *[[Ileon - Anatomía & Fisiología|Ileon]] |
| − | |||
====Desarrollo==== | ====Desarrollo==== | ||
| − | + | The small intestine develops from the digestive tube, which exists ventrally in the developing embryo. The digestive tube is endoderm, and therefore the small intestine and it's associated glands develop primarily from endoderm. Splanchnic mesoderm surrounds the digestive tube and gives rise to muscles of the tunica muscularis (for peristalsis), blood vessels in the submucosa and connective tissue of the serosa. | |
| − | + | The intestines begin as a straight tube, suspended by the dorsal mesentry. The midgut and mesentry elongate to form a loop. The descending limb of the loop will form the [[Duodeno - Anatomía & Fisiología|duodeno]], [[Yeyuno - Anatomía & Fisiología|yeyuno]] and [[Ileon - Anatomía & Fisiología|ileum]]. The ascending limb will form the terminal portion of the [[Ileon - Anatomía & Fisiología|ileum]], [[Ciego - Anatomía & Fisiología|ciego]] and first half of the [[Colon - Anatomía & Fisiología|colon]]. The midgut loop rotates about the cranial mesenteric artery in a clockwise direction (when viewed dorsoventrally). It undergoes a 270° rotation so that the [[Ciego - Anatomía & Fisiología|ciego]] and ascending [[Colon - Anatomía & Fisiología|colon]] ends up on the right, and the small intestine ends up on the left. | |
==Estructura== | ==Estructura== | ||
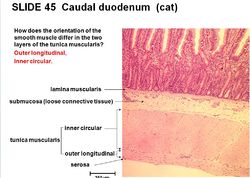
| − | + | The small intestine is attached along it's whole length to the dorsal abdominal wall by [[Cavidad Peritoneal - Anatomía & Fisiología|mesentery]]. The [[Cavidad Peritoneal - Anatomía & Fisiología|mesentery]] is relatively long for its most part, giving the small intestine a great deal of mobility. The basic structure of the intestinal wall is conserved throughout the whole length of the alimentary tract, but there is greatest diversity in the epithelial layer. Within the tunica muscularis are muscles present for peristalis and mixing of food. There are two muscle layers; an inner circular and outer longitudinal layer. Between the two muscle layers is the '''myenteric plexus'''. Between the inner circular layer of muscle in the tunica muscularis and the submucosa is the '''submucosal plexus'''. (see [[#Regulation & Control|regulation and control]]). | |
| − | == | + | ==Function== |
| − | === | + | ===To mix content and transport chyme=== |
| − | [[Image:tunica muscularis.jpg|thumb|right|250px| | + | [[Image:tunica muscularis.jpg|thumb|right|250px|Orientation of muscle in the tunica muscularis- © RVC 2008]] |
| − | + | Contraction of the two muscle layers facilitates mixing and transportation. There are two types of muscle contraction: | |
| − | |||
| − | |||
| − | + | '''Segmental''' | |
| − | '' | + | Rhythmic contraction of ''circular muscle'', creates ring like contractions. It divides content into many segments and moves segments backwards and forth causing mixing with digestive juices. This type of contraction predominates during digestion. |
| − | + | '''Peristaltic''' | |
| − | === | + | Antagonistic contraction of longitudinal ''and'' circular muscle. Transports chyme through the small intestine but contractions can be weak to allow time for absorption. When a peristaltic ‘’wave’’ of contraction reaches the end of the [[Ileon - Anatomía & Fisiología|ileum]], another starts in the [[Duodeno - Anatomía & Fisiología|duodeno]]. This is known as a ''migrating myoelectric complex''. |
| + | |||
| + | ===To secrete enzymes for the digestion of chyme and absorb the products of digestion=== | ||
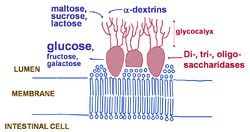
[[Image:Dissacharidase.jpg|thumb|right|250px|Dissacharidase - © RVC 2008]] | [[Image:Dissacharidase.jpg|thumb|right|250px|Dissacharidase - © RVC 2008]] | ||
| − | |||
| − | ==== | + | In digestion, large, complex molecules are broken down into their constituents. They are then absorbed and used by the body for energy or used as building blocks for new complex molecules. The three main molecules that undergo digestion are [[#Carbohydrate Digestion and Absorption|carbohydrates]], [[#Triacylglycerol Digestion and Absorption|triacyglycerols]] and [[#Protein Digestion and Absorption|proteins]]. |
| + | |||
| + | ====Carbohydrate Digestion and Absorption==== | ||
| − | The main soluble carbohdrates found in food are starch, found mainly in plants, and glycogen, found mainly in animal meat. There are two types of starch, ''amylose'' which has α1-4 glycosidic links and, ''amylopectin'' which has α1-4 glycosidic links and α1-6 glycosidic links making it branched (branches every glucose 25 residues). ''Glycogen'' is synthesised in the [[Hígado - Anatomía & Fisiología|hígado]] and [[ | + | The main soluble carbohdrates found in food are starch, found mainly in plants, and glycogen, found mainly in animal meat. There are two types of starch, ''amylose'' which has α1-4 glycosidic links and, ''amylopectin'' which has α1-4 glycosidic links and α1-6 glycosidic links making it branched (branches every glucose 25 residues). ''Glycogen'' is synthesised in the [[Hígado - Anatomía & Fisiología|hígado]] and [[Muscles - Anatomía & Fisiología|muscle]] and is similar to amylopectin as it has both α1-4 glycosidic links and α1-6 glycosidic links. However, it is more highly branched with shorter branches (branches every 12-18 glucose residues). |
| − | The '''first stage''' of carbohydrate digestion begins with α-amylase, which is an endoglycosidase. ''(This means it breaks bonds in the middle of the polymer to produce di-, tri- and oligo-saccharides).'' α-Amylase is present in [[ | + | The '''first stage''' of carbohydrate digestion begins with α-amylase, which is an endoglycosidase. ''(This means it breaks bonds in the middle of the polymer to produce di-, tri- and oligo-saccharides).'' α-Amylase is present in [[Salivary Glands - Anatomía & Fisiología|saliva]]. Salivary α-amylase is inactivated when it enters the [[Estómago Monogástrico - Anatomía & Fisiología|stomach]] due to it's acidic pH. |
| − | Carbohydrate digestion continues in the lumen of the [[Intestino Delgado - Resumen - | + | Carbohydrate digestion continues in the lumen of the [[Intestino Delgado - Resumen - Anatomy & Physiology|intestino delgado]] as pancreatic α-amylase enters the [[Duodeno - Anatomía & Fisiología|duodeno]] in the pancreatic duct. This is the site of the majority of carbohydrate digestion. The '''second stage''' is the digestion of di-, tri-, and oligo-saccharides to monosaccharides. This is done by di-, tri-, and oligo-saccharidases which have a glycocalyx to trap their substrate. They are bound to enterocytes. The main dissacharides that are broken down are; Maltose into two glucose molecules, sucrose into a glucose and fructose molecule and lactose into a glucose and galactose molecule. These monomers can then be absorbed. |
Absorption of glucose and galactose is coupled to sodium absorption and occurs through a symport called SGLT-1. Sodium potassium pumps in the enterocyte plasma membrane pump sodium out of the cell so that there is a higher concentration in the intestinal lumen than in the enterocyte. There is a net negative charge on the cell. Sodium diffuses down it's concentration and electrochemical gradient back into the enterocyte through the symport. This releases some energy. The energy release is used to transport glucose and galactose up their concentration gradients into the enterocyte. Glucose and galactose can then diffuse into the blood (portal vein) by carrier mediated diffusion via a GLUT-5 transporter. | Absorption of glucose and galactose is coupled to sodium absorption and occurs through a symport called SGLT-1. Sodium potassium pumps in the enterocyte plasma membrane pump sodium out of the cell so that there is a higher concentration in the intestinal lumen than in the enterocyte. There is a net negative charge on the cell. Sodium diffuses down it's concentration and electrochemical gradient back into the enterocyte through the symport. This releases some energy. The energy release is used to transport glucose and galactose up their concentration gradients into the enterocyte. Glucose and galactose can then diffuse into the blood (portal vein) by carrier mediated diffusion via a GLUT-5 transporter. | ||
| − | ==== | + | ====Triacylglycerol Digestion and Absorption==== |
| − | Triacylglycerols (TAGs) are digested by lipases. TAG digestion begins in the [[Cavidad Oral - Resumen - Anatomía & Fisiología|cavidad oral]], where lingual lipase is secreted in the [[ | + | Triacylglycerols (TAGs) are digested by lipases. TAG digestion begins in the [[Cavidad Oral - Resumen - Anatomía & Fisiología|cavidad oral]], where lingual lipase is secreted in the [[Salivary Glands - Anatomía & Fisiología|saliva]]. It removes a fatty acid from the 3 position on the glycerol molecule producing 1,2-diacylglycerol(1,2 DAG) and a free fatty acid. TAG digestion continues in the small intestine, with pancreatic lipase and bile from the [[Hígado - Anatomía & Fisiología|hígado]]. Pancreatic lipase is water soluble and the TAG and 1,2-DAG are lipid soluble. Bile creates an interface for the enzyme to digest the lipid molecules. Bile also emulsifies fats; it reduces the size of lipid droplets increasing the surface area available for digestion. Pancreatic lipase removes any further fatty acids from the 3 position and then from the 1 position to produce 2-monoacylglycerol (2-MAG) and a fatty acid. Pancreatic lipase is unable to remove the fatty acid from the 2 position, so an enzyme called '''isomerase''' transfers the fatty acid from the 2 postion to the 1 postion to produce 1-monoacylglycerol (1-MAG). Pancreatic lipase can then remove the fatty acid from the 1 position to produce a fatty acid and glycerol. |
''NB: Pancreatic lipase works quickly, whilst isomerase works slowly. Thus, 2-MAG often accumulates and is absorbed (70% of digested TAG are absorbed as 2-MAG). A small proportion is absorbed as 1-MAG (6%).'' | ''NB: Pancreatic lipase works quickly, whilst isomerase works slowly. Thus, 2-MAG often accumulates and is absorbed (70% of digested TAG are absorbed as 2-MAG). A small proportion is absorbed as 1-MAG (6%).'' | ||
| Línea 55: | Línea 55: | ||
The products of TAG digestion diffuse passively into the enterocyte as they are lipid soluble. They are then recombined to produce TAG. Fatty acids are converted to fatty acyl CoA by the addition of CoA. Fatty acyl CoAs are then added successively to 2-MAG to produce a TAG. In the golgi apparatus, TAG are then packaged with proteins, phospholipid and cholesterol into lipoproteins called '''chylomicrons'''. Chylomicrons are too large to enter the capillaries but instead enter the lymph to eventually join the blood via the thoracic duct. This enables the lipid soluble TAG to be transported in the blood. | The products of TAG digestion diffuse passively into the enterocyte as they are lipid soluble. They are then recombined to produce TAG. Fatty acids are converted to fatty acyl CoA by the addition of CoA. Fatty acyl CoAs are then added successively to 2-MAG to produce a TAG. In the golgi apparatus, TAG are then packaged with proteins, phospholipid and cholesterol into lipoproteins called '''chylomicrons'''. Chylomicrons are too large to enter the capillaries but instead enter the lymph to eventually join the blood via the thoracic duct. This enables the lipid soluble TAG to be transported in the blood. | ||
| − | ==== | + | ====Protein Digestion and Absorption==== |
| − | Protein digestion begins in the [[Estómago Monogástrico - | + | Protein digestion begins in the [[Estómago Monogástrico - Anatomy & Physiology|stomach]] where pepsin is secreted as a zymogen, pepsinogen. Pepsin is an endopeptidase and produces smaller polypeptides. Pepsin prefers to break peptide bonds of larger polypeptides, where there is a large hydrophobic amino acid on the N-terminal side. Protein digestion continues in the small intestine. There are three endopeptidases in the small intestine; trypsin; chymotrypsin; and elastase. They are all secreted as zymogens; inactive precursors. |
Trypsin is secreted as trypsinogen, chymotrypsin is secreted as chymotrypsinogen and elastase is secreted as proelastase. Trypsinogen is initially activated by enterokinase (activation involves the cleavage of 6 amino acids). Trypsinogen can then activate itself, and also chymotrypsin and elastase. The short polypeptides produced from their digestion are further digested by exopeptidases which remove amino acids from the end of the polypeptide chain. | Trypsin is secreted as trypsinogen, chymotrypsin is secreted as chymotrypsinogen and elastase is secreted as proelastase. Trypsinogen is initially activated by enterokinase (activation involves the cleavage of 6 amino acids). Trypsinogen can then activate itself, and also chymotrypsin and elastase. The short polypeptides produced from their digestion are further digested by exopeptidases which remove amino acids from the end of the polypeptide chain. | ||
| Línea 73: | Línea 73: | ||
Amino acids within the same group compete with each other for the transport molecule. Amino acids are transported with sodium through a symport (like glucose), where amino acids travel up their concentration gradient and sodium travels down its concentration gradient. Di-,tri- and oligo- peptides are absorbed by the γ glutamyl transfer cycle. γ Glutamyl transferase spans the enterocyte membrane and combines glutathione from the inside of the cell with a di-,tri- or oligo-peptide from the intestinal lumen forming a γ-glu-aa complex which is transported into the cell. The aas are then released and glutathione is recombined to enter the process again. | Amino acids within the same group compete with each other for the transport molecule. Amino acids are transported with sodium through a symport (like glucose), where amino acids travel up their concentration gradient and sodium travels down its concentration gradient. Di-,tri- and oligo- peptides are absorbed by the γ glutamyl transfer cycle. γ Glutamyl transferase spans the enterocyte membrane and combines glutathione from the inside of the cell with a di-,tri- or oligo-peptide from the intestinal lumen forming a γ-glu-aa complex which is transported into the cell. The aas are then released and glutathione is recombined to enter the process again. | ||
| − | == | + | ==Regulation & Control== |
The functions of the small (and large) intestine are regulated by three mechanisms: Endocrine hormones, paracrine hormones and neural transmitters. Unlike the [[Estómago Monogástrico - Anatomía & Fisiología|stomach]], control is mainly local, with superimposed co-ordination through the extrinsic ANS. All signals affect the small intestine via sensory neurones. Neurones interact with two plexuses in the intestinal wall. Neurones in the ''myenteric plexus'' produce changes in muscle ''contractility''. Neurones in the ''submucosal plexus'' produce changes in ''secretion'' and ''blood flow'' to the small intestine. Plexuses are connected via interneurones. | The functions of the small (and large) intestine are regulated by three mechanisms: Endocrine hormones, paracrine hormones and neural transmitters. Unlike the [[Estómago Monogástrico - Anatomía & Fisiología|stomach]], control is mainly local, with superimposed co-ordination through the extrinsic ANS. All signals affect the small intestine via sensory neurones. Neurones interact with two plexuses in the intestinal wall. Neurones in the ''myenteric plexus'' produce changes in muscle ''contractility''. Neurones in the ''submucosal plexus'' produce changes in ''secretion'' and ''blood flow'' to the small intestine. Plexuses are connected via interneurones. | ||
| Línea 138: | Línea 138: | ||
==Enlaces== | ==Enlaces== | ||
| − | '''Test yourself with the [[ | + | '''Test yourself with the [[Small Intestine - Anatomy & Physiology - Flashcards|Small Intestine Flashcards]]''' |
'''Click here for information on [[Peyer's Patches - Anatomy & Physiology|Peyer's Patches]]''' | '''Click here for information on [[Peyer's Patches - Anatomy & Physiology|Peyer's Patches]]''' | ||
Revisión del 12:29 7 may 2011
Introduction
The small intestine extends from the pylorus of the stomach to the ciego. The small intestine recieves chyme from the stomach. It is the main site of chemical degradation and absorption of chyme. Fats are exclusively broken down in this part of the alimentary tract. Carbohydrates and proteins that are not degraded in the small intestine are available for microbial fermentation in the intestino grueso. The small intestine produces enzymes for digestion of protein, carbohydrate and fat and absorbs the products of their digestion. Enzymes are produced by glands in the intestinal wall and the páncreas. The vesícula biliar produces bile which emulsifies fats for digestion. Absorption is facilitated by ridges in the small intestine and by the presence of villi and microvilli.
The small intestine consists of three parts. Each part differs in anatomy, but all have the same basic structure and function:
Desarrollo
The small intestine develops from the digestive tube, which exists ventrally in the developing embryo. The digestive tube is endoderm, and therefore the small intestine and it's associated glands develop primarily from endoderm. Splanchnic mesoderm surrounds the digestive tube and gives rise to muscles of the tunica muscularis (for peristalsis), blood vessels in the submucosa and connective tissue of the serosa.
The intestines begin as a straight tube, suspended by the dorsal mesentry. The midgut and mesentry elongate to form a loop. The descending limb of the loop will form the duodeno, yeyuno and ileum. The ascending limb will form the terminal portion of the ileum, ciego and first half of the colon. The midgut loop rotates about the cranial mesenteric artery in a clockwise direction (when viewed dorsoventrally). It undergoes a 270° rotation so that the ciego and ascending colon ends up on the right, and the small intestine ends up on the left.
Estructura
The small intestine is attached along it's whole length to the dorsal abdominal wall by mesentery. The mesentery is relatively long for its most part, giving the small intestine a great deal of mobility. The basic structure of the intestinal wall is conserved throughout the whole length of the alimentary tract, but there is greatest diversity in the epithelial layer. Within the tunica muscularis are muscles present for peristalis and mixing of food. There are two muscle layers; an inner circular and outer longitudinal layer. Between the two muscle layers is the myenteric plexus. Between the inner circular layer of muscle in the tunica muscularis and the submucosa is the submucosal plexus. (see regulation and control).
Function
To mix content and transport chyme
Contraction of the two muscle layers facilitates mixing and transportation. There are two types of muscle contraction:
Segmental
Rhythmic contraction of circular muscle, creates ring like contractions. It divides content into many segments and moves segments backwards and forth causing mixing with digestive juices. This type of contraction predominates during digestion.
Peristaltic
Antagonistic contraction of longitudinal and circular muscle. Transports chyme through the small intestine but contractions can be weak to allow time for absorption. When a peristaltic ‘’wave’’ of contraction reaches the end of the ileum, another starts in the duodeno. This is known as a migrating myoelectric complex.
To secrete enzymes for the digestion of chyme and absorb the products of digestion
In digestion, large, complex molecules are broken down into their constituents. They are then absorbed and used by the body for energy or used as building blocks for new complex molecules. The three main molecules that undergo digestion are carbohydrates, triacyglycerols and proteins.
Carbohydrate Digestion and Absorption
The main soluble carbohdrates found in food are starch, found mainly in plants, and glycogen, found mainly in animal meat. There are two types of starch, amylose which has α1-4 glycosidic links and, amylopectin which has α1-4 glycosidic links and α1-6 glycosidic links making it branched (branches every glucose 25 residues). Glycogen is synthesised in the hígado and muscle and is similar to amylopectin as it has both α1-4 glycosidic links and α1-6 glycosidic links. However, it is more highly branched with shorter branches (branches every 12-18 glucose residues). The first stage of carbohydrate digestion begins with α-amylase, which is an endoglycosidase. (This means it breaks bonds in the middle of the polymer to produce di-, tri- and oligo-saccharides). α-Amylase is present in saliva. Salivary α-amylase is inactivated when it enters the stomach due to it's acidic pH.
Carbohydrate digestion continues in the lumen of the intestino delgado as pancreatic α-amylase enters the duodeno in the pancreatic duct. This is the site of the majority of carbohydrate digestion. The second stage is the digestion of di-, tri-, and oligo-saccharides to monosaccharides. This is done by di-, tri-, and oligo-saccharidases which have a glycocalyx to trap their substrate. They are bound to enterocytes. The main dissacharides that are broken down are; Maltose into two glucose molecules, sucrose into a glucose and fructose molecule and lactose into a glucose and galactose molecule. These monomers can then be absorbed.
Absorption of glucose and galactose is coupled to sodium absorption and occurs through a symport called SGLT-1. Sodium potassium pumps in the enterocyte plasma membrane pump sodium out of the cell so that there is a higher concentration in the intestinal lumen than in the enterocyte. There is a net negative charge on the cell. Sodium diffuses down it's concentration and electrochemical gradient back into the enterocyte through the symport. This releases some energy. The energy release is used to transport glucose and galactose up their concentration gradients into the enterocyte. Glucose and galactose can then diffuse into the blood (portal vein) by carrier mediated diffusion via a GLUT-5 transporter.
Triacylglycerol Digestion and Absorption
Triacylglycerols (TAGs) are digested by lipases. TAG digestion begins in the cavidad oral, where lingual lipase is secreted in the saliva. It removes a fatty acid from the 3 position on the glycerol molecule producing 1,2-diacylglycerol(1,2 DAG) and a free fatty acid. TAG digestion continues in the small intestine, with pancreatic lipase and bile from the hígado. Pancreatic lipase is water soluble and the TAG and 1,2-DAG are lipid soluble. Bile creates an interface for the enzyme to digest the lipid molecules. Bile also emulsifies fats; it reduces the size of lipid droplets increasing the surface area available for digestion. Pancreatic lipase removes any further fatty acids from the 3 position and then from the 1 position to produce 2-monoacylglycerol (2-MAG) and a fatty acid. Pancreatic lipase is unable to remove the fatty acid from the 2 position, so an enzyme called isomerase transfers the fatty acid from the 2 postion to the 1 postion to produce 1-monoacylglycerol (1-MAG). Pancreatic lipase can then remove the fatty acid from the 1 position to produce a fatty acid and glycerol.
NB: Pancreatic lipase works quickly, whilst isomerase works slowly. Thus, 2-MAG often accumulates and is absorbed (70% of digested TAG are absorbed as 2-MAG). A small proportion is absorbed as 1-MAG (6%).
The products of TAG digestion diffuse passively into the enterocyte as they are lipid soluble. They are then recombined to produce TAG. Fatty acids are converted to fatty acyl CoA by the addition of CoA. Fatty acyl CoAs are then added successively to 2-MAG to produce a TAG. In the golgi apparatus, TAG are then packaged with proteins, phospholipid and cholesterol into lipoproteins called chylomicrons. Chylomicrons are too large to enter the capillaries but instead enter the lymph to eventually join the blood via the thoracic duct. This enables the lipid soluble TAG to be transported in the blood.
Protein Digestion and Absorption
Protein digestion begins in the stomach where pepsin is secreted as a zymogen, pepsinogen. Pepsin is an endopeptidase and produces smaller polypeptides. Pepsin prefers to break peptide bonds of larger polypeptides, where there is a large hydrophobic amino acid on the N-terminal side. Protein digestion continues in the small intestine. There are three endopeptidases in the small intestine; trypsin; chymotrypsin; and elastase. They are all secreted as zymogens; inactive precursors.
Trypsin is secreted as trypsinogen, chymotrypsin is secreted as chymotrypsinogen and elastase is secreted as proelastase. Trypsinogen is initially activated by enterokinase (activation involves the cleavage of 6 amino acids). Trypsinogen can then activate itself, and also chymotrypsin and elastase. The short polypeptides produced from their digestion are further digested by exopeptidases which remove amino acids from the end of the polypeptide chain.
There are two types of exopeptidase in the small intestine: carboxypeptidases' that split amino acids off the polypeptide from the C-terminus. Produced by the pancreas as zymogens that also become activated by trypsin. Aminopeptidases that split amino acids off the polypepetide from the N-terminus are produced by the small intestine (not as zymogens). The final products of protein digestion are amino acids and some di-,tri- and oligo-peptides. Amino acids are absorbed by four carrier proteins; each transports a different type of amino acid.
1. Neutral amino acids e.g. alanine, valine, leucine.
2. Dibasic amino acids e.g. lysine, arginine.
3. Acidic amino acids e.g. glutamine, aspartic acid.
4. Small amino acids inc. proline, hydroxyproline and glycine.
Amino acids within the same group compete with each other for the transport molecule. Amino acids are transported with sodium through a symport (like glucose), where amino acids travel up their concentration gradient and sodium travels down its concentration gradient. Di-,tri- and oligo- peptides are absorbed by the γ glutamyl transfer cycle. γ Glutamyl transferase spans the enterocyte membrane and combines glutathione from the inside of the cell with a di-,tri- or oligo-peptide from the intestinal lumen forming a γ-glu-aa complex which is transported into the cell. The aas are then released and glutathione is recombined to enter the process again.
Regulation & Control
The functions of the small (and large) intestine are regulated by three mechanisms: Endocrine hormones, paracrine hormones and neural transmitters. Unlike the stomach, control is mainly local, with superimposed co-ordination through the extrinsic ANS. All signals affect the small intestine via sensory neurones. Neurones interact with two plexuses in the intestinal wall. Neurones in the myenteric plexus produce changes in muscle contractility. Neurones in the submucosal plexus produce changes in secretion and blood flow to the small intestine. Plexuses are connected via interneurones.
Excitatory neurotransmitters of the parasympathetic nervous system include: substance P, acetylcholine (via muscarinic M1 and M2 receptors) and serotonin (5-HT).
Inhibitory (sympathomimetic) neurotransmitters include: vasoactive intestinal polypeptide (VIP), nitric oxide (NO), ATP and enkephalins.
The autonomic nervous system (ANS) control is superimposed over local control. The small intestine recieves sympathetic and parasympathetic innervation, which act via the same two plexuses. Parasympathetic innervation stimulates motility and secretion, Sympathetic innervation antagonises the parasympathetic nervous system and inhibits motility and secretion. Sympathetic neurones have coeliac, cranial mesenteric and caudal mesenteric ganglia at the corresponding branches of the aorta. As the sympathetic fibres leave the ganglia, they surround the respective artery. Generation of action potentials is intrinsic to the smooth muscle in the intestine.
Interstitial cells of Cajal act as muscle pacemakers and generate a basic electrical rhythm (BER). The BER is able to pass between cells due to the presence of gap junctions. The muscle therefore acts as a syncytium. Some BER are sufficient to generate an action potential. Food in the intestine stimulates peristalsis to occur, and increases the likelihood of an action potential occuring. Enteroendcrine cells in the crypts of the small intestine produce substances that profoundly influence GIT motility. Hormones produced by enteroendocrine cells in the small intestine include; secretin; gastric inhibitory peptide; and gastrin.
Lymphatics
The products of fat digestion are transported in the lymph via the lymphatic vessels, and when fat has been absorbed, it turns the lymph a milky colour. Lymph travels to the mesenteric lymph nodes and then through the efferent vessels that converge to form the cranial mesenteric trunk. The cranial mesenteric trunk drains into the chyle cistern. This is a dilation of the thoracic duct at its origin. It lies dorsally to the aorta and extends from the diaphragmatic crura to the renal arteries. Flow of lymph is facilitated by movement of the diaphragm in ventilation of the lungs and by pulsation of the aorta.
Diferencias Entre las Species
In the dog, mesenteric lymph nodes are found mainly around the root of the mesentry. In the pig, they form a long raised band in the middle of the mesentry. They are routinely examined after slaughter as enlargement indicates enteric disease or tuberculosis.
Carnivore
Relatively short intestine; in dogs it is approximately three times the body length.
Equino
25m in the carcass (in life the figure is much less).
Ovino
Up to 25 times body length.
Bovino
Up to 50m.
Histología
- The mucosa is arranged into villi that provide a large surface area for absorption.
- Epithelium is simple columnar - ideal for absorption.
- Epithelial cells are known as enterocytes.
- A single layer of enterocytes overlies the lamina propria.
- Enterocytes originate from progenitor cells that migrate from mucosal crypts. They differentiate as they migrate up the villus.
- Enterocytes are absorptive and posses microvilli.
- Membrane bound enzymes and transport proteins are also within the epithelium.
- Each villus houses a generous blood supply of capillaries that transport amino acids, monosaccharides and other digestive products and lacteals that transport triacylglycerides. Lacteals drain into the lymphatic system.
- Two types of secretion are produced in the small intestine; together they are called the succus entericus. The first type of secretion is from the crypts, the second is from the Brunner's glands.
- Crypts are present at the base of each villus in the mucosa. Cell types in mucosal crypts (from luminal to basal):
- goblet at the tip of the crypt. Produce mucous by exocytosis.
- entero-endocrine in the middle of the crypt. Produce many important substances for the regulation of GIT motility. See Regulation & Control.
- paneth at the base of the crypt. Function unknown. Contain eosinophilic granules.
- Lamina muscularis is smooth muscle.
- Brunner's glands are present in the submucosa of the duodenum.
- Secrete a protective mucous.
- Produce an alkaline secretion which neutralises stomach acid.
- Open into the crypts in the mucosa above.
- Contraction of smooth muscle shortens the villus. This helps to pump out absorbed products of digestion. Relaxation of smooth muscle lengthens the villus which increases surface area, facilitating absorption.
- Submucosa is loose connective tissue and it contains blood vessels and nerve fibres.
- Tunica muscularis is smooth muscle.
- It consists of two muscle layers (see regulation & control).
- An inner circular layer
- An outer longitudinal layer
- It consists of two muscle layers (see regulation & control).
- Serosa is loose connective tissue.
Enlaces
Test yourself with the Small Intestine Flashcards
Click here for information on Peyer's Patches
Click here for information on Pathology of the Small and Large Intestines
Click here for information on The Horse's Small Intestine
Enlaces de Video:
Pot 48 The Small and Large intestine of the Ruminant
Lateral View of the Equine Abdomen
Left Sided topography of the Equine abdomen
Right sided topography of the Equine Abdomen
Small and Large intestine of the Sheep